Understanding
Basal-Bolus
Learn more
Designing Your Insulin Dosing Regimen
Learn moreNavigating
Insulin Math
Learn more
With today’s newer analogue designer insulins, we can replace insulin in such a way that it is fairly physiologic. In other words, the newer insulins match what the body would have done if the body could have done it. Basal insulins have an extended insulin release giving a flat basal profile, excellent to mimic the basal insulin the body would have made for glucose produced by the liver. Additionally, rapid analog insulins peak quickly to match the glucose absorbed at meals.
Basal
A long-acting Insulin with a flat profile that lasts >24 hours. Basal is meant to meet fasting insulin needs. Normally, endogenous basal insulin from the pancreas and glucose from the liver are always being made and is required for living, whether the person is eating not. Therefore in relative insulin deficiency (type 2 diabetes) or with absolute insulin deficiency (type 1 diabetes), replacing basal insulin is essential.
Bolus
A rapid acting insulin, which generally peaks within an hour and is mostly finished in 2-4 hours. The quick peak is meant to handle glucose absorbed at a meal. All type 1 patients and some patients with type 2 diabetes have lost the ability to mount an insulin response to a meal. These patients will require bolus insulin.
A BASAL-BOLUS Analogy
Suppose you have to travel three days across a desert. Where will the glucose come from to give you the energy needed to make it across the desert? Answer: You either eat it, make it, or break it down.
Blood glucose sources:
- Food- Glucose is absorbed by the gut upon carbohydrate ingestion
- Gluconeogenesis- Glucose production by the liver and kidneys.
- Glycogenolysis- breakdown of the body’s glucose stores
Without food in the middle of the desert, energy must come from the liver or kidneys from either glucose breakdown or glucose production. This glucose fulfills fasting energy requirements. Insulin that utilizes fasting glucose is called BASAL insulin and without it, glucose will remain in the bloodstream.
Additionally, if in the middle of the desert if you find & eat a coconut, you will get a large BOLUS of glucose all at once. Your pancreas will need to BOLUS or give quick rapid acting insulin to match the rapidly absorbing glucose you’ve just ingested. This BOLUS insulin will allow the glucose from your food to enter your cells where it can be used, thus helping to maintain a normal blood glucose concentration.

You must think like a pancreas. When replacing insulin, you must give Basal and Bolus insulin like the body would have, if it could have.
BASAL-BOLUS Components & How To Use Them
BASAL Insulin
Basal insulin should deliver a consistent level of insulin to the bloodstream to match the glucose being produced by the body, or in other words, it must balance. Too much basal will predispose patients to hypoglycemia in a fasting state (like when sleeping). Too little basal will lead to gradual hyperglycemia and poor control.
Conceptual image for basal insulin replacement
Choosing your basal insulin type largely depends on which insulin is covered by the patient's insurance. Most basal insulins do the job, but there are some nuances to consider. The chart below describes the various BASAL insulins and might help you to decide which might work best for your patients.
Long Acting Basal Insulin Types
| Brand | Duration | Description | |
|---|---|---|---|
| Basaglar (glargine) | Peakless ~24 hours | Biosimilar to Lantus. Dosed daily. | |
| Lantus (glargine) | Peakless. ~24 hours | Dosed daily | |
| Levemir (detemir) | Dose dependant | Dosed twice daily. At lower doses (u/kg) lasts <24 hours. | |
| Toujeo (U300 glargine) | ~5 days to steady state | Dosed daily. Ultra long acting concentrated glargine that gives a protracted duration of 72 hours with very flat profile. ~20% weaker than glargine U100. Only comes in pens | |
| Tresiba (degludec) U100 or U200 | ~3-4 days to steady state | Dosed daily. Ultra long acting. For larger doses the U200 concentration injects less volume per dose. | |
| Combination GLP1-A with Basal Insulin | |||
| Soliqua (glargine + lixisenatide (GLP-1 Agonist) | glargine ~24 hours. lixisenatide ½-life ~3 hours. |
lixisenatide is a GLP1-Agonist. With a short duration and a maximal effect near 2.5-3 hours. For this reason, dosing before breakfast and dinner is helpful, or the biggest meal of the day. | |
| Xultophy (degludec + liraglutide) | glargine ~24 hours liraglutide |
liraglutide is a GLP-1-Agonist with ~24 hour duration. Dosed daily. | |
Calculating Basal Insulin Dose
Basal insulin dosage varies widely. Factors such as body weight, activity level, types of foods, amount of endogenous insulin, etc. all play a role. For full insulin replacement, it is generally about 50% of the patient’s expected Total Daily Dose (TDD), however if your patient needs basal insulin alone, you may consider starting with 0.1-0.2 u/kg/day. See Navigating Insulin Math for specific dosing recommendations and examples.
Bolus Doses
A rapid acting insulin is given as a BOLUS primarily for two reasons: meals & high glucose correction.
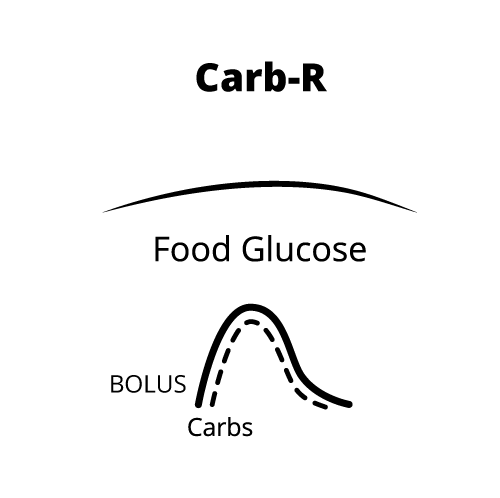
Food bolus: A rapid acting insulin is given premeal based on the carbohydrate intake. Once given, it is meant to absorb at the same rate the food is being digested into the bloodstream. This balance (if perfect) would keep the blood glucose flat with little to no glucose rise just like the body would have done if it could produce insulin at the onset of a meal. The insulin-carb (Carb-R) ratio is usually expressed as 1 unit of insulin for every x grams of carbohydrate consumed. Example: 1 unit/10 grams or 1u:10g or 1:10
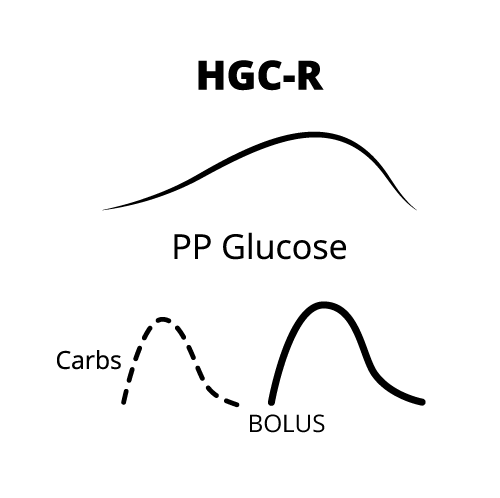
Correction bolus: A rapid acting insulin is also given when the glucose has risen above the target range. The High Glucose Correction Ratio (HGC-R) signifies that 1 unit of insulin will drop the blood glucose a certain number of points. Example: A 1:30 ratio, means 1 unit of insulin will drop the BG 30 points. A target is set to where you’d like the glucose to fall, like 120 mg/dL for example. This can be expressed as: 1 units per 30 point BG>120 or 1/30 points>120 or 1:30>120
Dosing math: Bolus ratios are determined by using two Rules of Thumb:
- The 1700 rule for the correction ratio &
- The 550 rule for the carbohydrate ratio.
Click here to the Navigating Insulin Math section for a more detailed explanation.
Below you will find mostly commonly used bolus insulin types.
Rapid Acting Insulin Types
| Brand | Onset | Peak | Duration |
|---|---|---|---|
| Amdelog (lispro) | ~60 min | ~60 min | ~2-4 hours |
| Apidra (glulisine) | ~15 min | ~60 min | ~2-4 hours |
| Fiasp (aspart) | ~12-14 min | ~40 min | ~3-5 hours |
| Humalog (lispro) U100 or U200 | ~60 min | ~60 min | ~2-4 hours |
| Novolog (aspart) | ~60 min | ~60 min | ~3-5 hours |
| Fast Acting | |||
| Humulin R, Novolin R (insulin regular human) | ~30-60 min | ~2-4 hours | ~6-8 hours |
| See pricing co-pay card spreadsheet for cost savings details | |||
Learn more about Designing Your Insulin Dosing Regimen in the next section.
