Understanding
Basal-Bolus
Learn more
Designing Your Insulin Dosing Regimen
Learn moreNavigating
Insulin Math
Learn more
When dosing insulin a provider must keep in mind the many variables that influence what a patient will require. Consider the following:
- Kidney function
- BMI
- Resting Metabolism
- Inflammation
- Appetite
- Illness
- Steroids
- Food types
- Hormones
- Stress
- Activity level
- etc.
No Magic Formula
Not all people will be "typical." Because patients are so individually different, there is no magical formula to dose insulin that worx perfectly for every patient every time. Below, you will find basic guidelines for dosing insulin, however ask for expert opinion if unfamiliar with dosing a particular insulin dosing regimen.
Disclaimer: InsulinWorx is for EDUCATIONAL PURPOSES ONLY. InsulinWorx elucidates on general insulin dosing guidelines, however does not recommend any one method of dosing insulin. Each patient is different and if you have any questions regarding dosing insulin, seek expert consultation.
General Recommendations for starting type 2 patients on insulin
AACE recommendations at a glance: Initiating Insulin in insulin naive patients.
| Basal | A1c <8% 0.1-0.2 u/kg/day A1c >8% 0.2-0.4 u/kg/day |
||
| Basal-Bolus | 0.3-0.5 u/kg/day (50% basal / 50% bolus) |
||
| Bolus Ratios | |||
| HGC-R | 1700 / TDD (units) | ||
| Carb-R | (550 / TDD) or (HGC-R / 3) | ||
| Bolus: Set Doses | (TDD x (30-50%)) / 3 | ||
| Remember the above guidelines are for starting doses. You will need to adjust the doses based on glycemic control. It is recommended you titrate insulin doses 10-20% for hyper or hypoglycemia every few days. *For any severe lows, decrease doses by 20-40% to keep patients safe. |
|||
How to initiate insulin in insulin-naive patients
When starting insulin there are many approaches as discussed in the Designing Your Insulin Dosing Regimen. Patient characteristics and preferences will guide where to begin. For type 2 patients whose fasting glucose values are elevated, simply adding a basal insulin may be the first step. If they have noticeable post-meal hyperglycemia, bolus injections should be considered. For type 1 patients, full insulin replacement is necessary.
Insulin dosing requirements vary broadly, however most patients will fall within 0.1 - 1.0 Total Daily Dose*. For starting patients initially on insulin, the American Association of Endocrinology (AACE) has given the following guidance:
For type 2 patients:
- If A1c <8%, consider starting basal insulin at 0.1-0.2 u/kg/day
- If A1c >8%, consider starting basal insulin at 0.2-0.4 units/day & possibly add bolus insulin.
- For basal and bolus insulins, AACE recommends a TDD of 0.3-0.5 u/kg/day as a good starting place.
For type 1 patients:
- For newly diagnosed type 1 patients, 0.4-0.5 TDD is a recommended starting place
Remember that with obesity, sedentary lifestyle or puberty insulin requirements may be much higher. For example, teenagers are often an exception to typical dosing. For lean, active kids who eat parents out of house and home, you will need much more bolus insulin. Additionally teens are growing. and insulin needs will commonly use as much as 1.5 units/kg/day. Growth hormones are a main contributing factor.
Additional Caveat- New onset type 1 diabetes patients would be best managed by someone trained in diabetes as a specialist. Type 1 patients is a lifelong condition that will have many variables which experts in the field can best address with the patient. A few variables include navigating the costs of insulin, pregnancy / pregnancy planning, how to adjust insulin in the honeymoon phase of diabetes or with dawn or somogyi phenomenons, work issues, exercise issues, devices including pumps and sensors, hypoglycemia instruction, concomitant conditions, complication screenings, and so forth.
Insulin Dosing Examples
Determining Basal Example
What would you do for a DM2 patient who weighs 200 lbs (91 kg), whose A1c is 8.0%, but is on 3 oral agents? Let’s say he consistently has fasting glucose values near 140 mg/dL.
According to the AACE guidelines, you may consider starting 0.1-0.2 u/kg/day of basal insulin and titrate 10-20% every few days until his fastings are less than 100 mg/dL while avoiding hypoglycemia.
Basal dose: 91kg x 0.2u/kg = 18 units
Determining Basal-Bolus Example
Let’s consider a DM2 patient who weighs 200 lbs (91 kg) whose A1c is 9.0% and is on 3 oral agents. His fastings are consistently near 180 mg/dL, but by the end of the day some glucose readings are near 270 mg/dL. In this example, basal alone will not cover his post-meal hyperglycemia. He needs additional bolus insulin.
According to the AACE guidelines, you may consider a TDD of 0.3-0.5 u/kg/day and split 50/50 for basal/bolus.
TDD: 91 kg x 0.5 u/kg/day = 45 units.
50% basal: 22
50% bolus: 22*
*You can divide the bolus doses evenly as set doses or use carb-counting (see below)
Remember, in the above example 0.5 u/kg/day is a starting dose and does not take into consideration the patient’s activity level, eating habits, kidney function, etc. The above dose may be too high or low depending on multiple factors. You may consider the recommended starting dose to be low for example, if this patient is starting on steroids and has a large appetite or too low if he has kidney disfunction and is not eating in a hospital bed.
Carbohydrate Counting Method:Go to Understanding BASAL-BOLUS for more information on Carbohydrate Counting
Two mathematical guidelines or rules are used for determining insulin boluses for food and correction:
- High Glucose Correction Ratio (HGC-R):
- 1700 Rule: 1700 / TDD
- Carbohydrate Ratio (Carb-R):
- 550 Rule: (550 / TDD) or
- (HGC-R)/3
**Different providers use different numbers, but these are used commonly.
If you’ve noticed, the 550 rule is about 1/3 of 1700. Thus once you determine your HGC-R, you can simply divide by 3 to get your Carb-R. (eg. HGC-R / 3 = Carb-R)
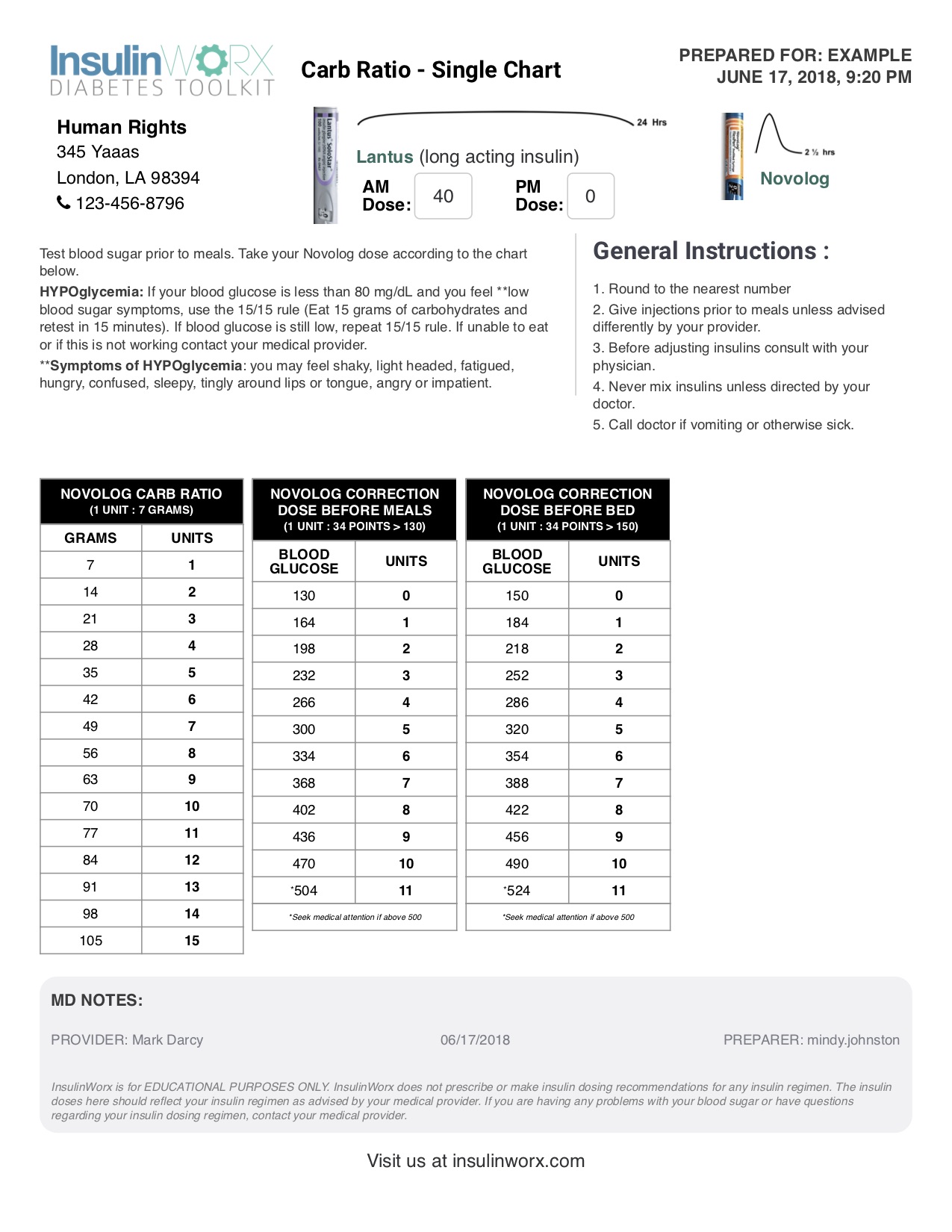
Carb-Counting Dosing Example
A patient weighs 220 lbs (100 kg) and has an average BG of 200 mg/dL. According to AACE guidelines, you might anticipate his full insulin requirements or TDD to be ~0.5 u/kg/day.
- TDD: 0.5 x 100 kg = 50 units
- BASAL: 50 units (TDD) x 50% = 25 units
- HGC-R: (1700 / 50 units (TDD))= 34 points (1 unit will lower BG about 34 points)
- CHO-R: (HGC/3) or (34 points / 3) = 11 (1 unit / 11 grams Carbs)
*Once again remember this is a starting place. More experienced providers may consider starting at a higher dose depending on the patient characteristics.
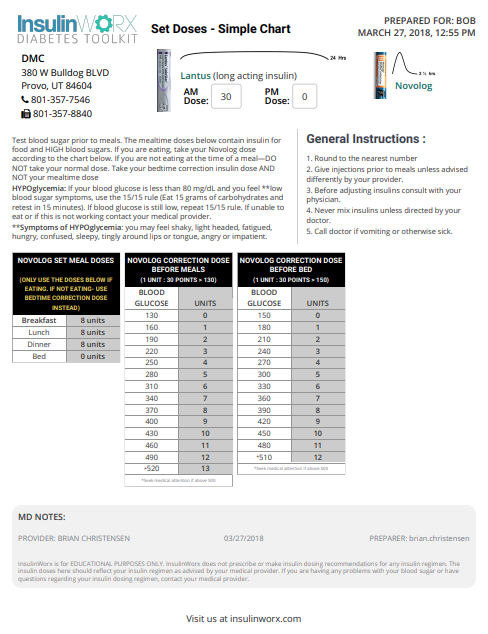
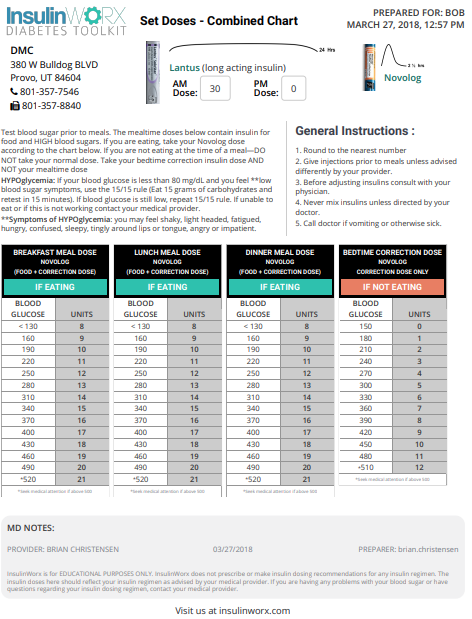
Set Doses Method
For Set Doses, you will calculate basal as you did before, but you will take 30-50% of TDD and divide it into the three meal boluses depending on appetite:
Meal Dose = (TDD x (30-50%)) / 3
Recall, this regimen is good for patients who typically eat a consistent amount of carbohydrates at each meal. If they want to skip a meal, they would not take a meal bolus, but may take a correction bolus if BG is elevated.
Dosing Example
Lets say this patient weighs 220 lbs or 100 kg and has a consistently high average BG of 260 mg/dL and an A1c if 10.8%. Let’s estimate they will need 0.6 u/kg/day to start. (Remember to consider your patient’s variables. If this was a hospital patient and his glucose average was 180, you might start at 0.3 u/kg/day TDD)
| TDD: | 100 kg x 0.6 u/kg/day = 60 units |
| Basal: | 50% x 60 units = 30 units |
| Bolus: | 40% x 60 units = 24 units |
| Meal dose: | 24 units / 3 meals = 8 units/meal |
| HGC-R: 1700/60 = | 1:30>130 (target BG) |
At a follow-up visit, if post-meal glucose values are high, consider titrating up by 10-20% until you obtain the desired glycemic control.
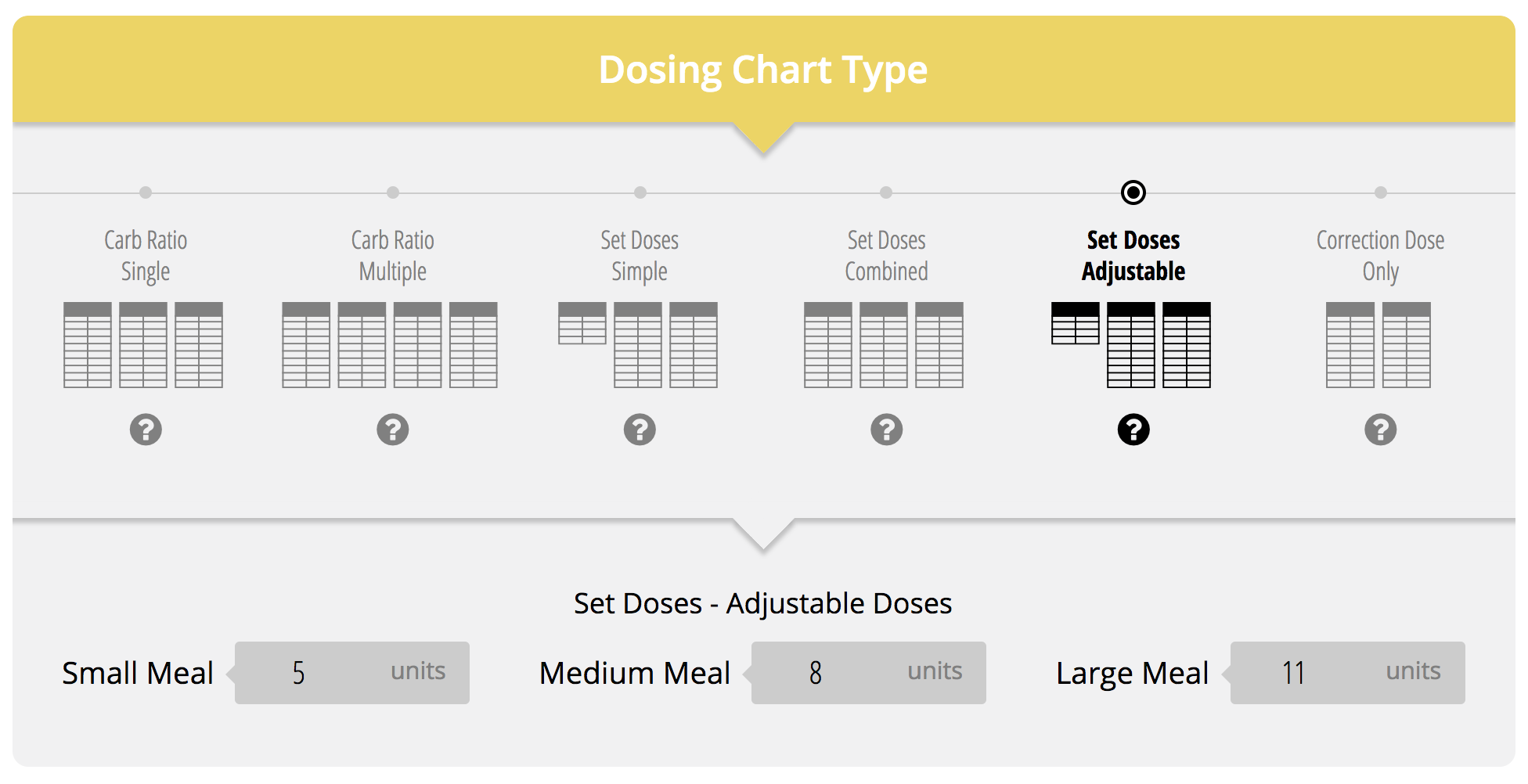
Adjustable Set Doses
Using the same example above, this same patient could have an adjustable set dose regimen.
Dosing Math:
| TDD: | 100 kg x 0.6 u/kg/day = 60 units |
| Basal: | 50% x 60 units = 30 units |
| Bolus: | 40% x 60 units = 24 units |
| Meal dose: | 24 units / 3 meals = 8 units/meal |
| HGC-R: 1700/60 = | 1:30>130 (target BG) |
If this patient was somewhat savvy and could adjust his/her dose according to the size of his meal, you could take the 8 unit dose, as estimated above, and estimate a few units either way for variable meal sizes. For example, he might have 5 units for a small meal, 8 for regular sized meal and 11 for a larger meal. It is important to get feedback from your patient however to see if you need more or less depending on their meal sizes.
Dosing for Mixed insulins (Hyperlink-regimen info)
Calculations
Mixed insulins, like BASAL-BOLUS regimens are also based on TDD.
According to AACE guidelines, you would take 0.3-0.5 u/kg/day TDD; however in this instance you would divided TDD into 2 doses at breakfast and dinner. Calculations are based on the rule of thirds:
- ⅔ of the TDD is given in the morning prior to breakfast.
- ⅓ of the TDD is given before dinner & will cover dinner and for overnight basal needs when they are not eating.
Dosing Example
A patient weighs 220 lbs or 100 kg with a glucose average of 255 mg/dL. Using 0.5 u/kg, let’s divide the insulin doses as follows
- TDD: 0.5 x 100 kg = 50 units
- ⅔ x 50 units = 33 units to be given at Breakfast
- ⅓ x 50 units = 16 units to be given at Dinner
Doses will be adjusted at subsequent visits to give the best estimation that will meet their carb intake needs. You may consider giving a HGC-R only chart to correct their high glucose levels, if they will use it alongside the mixed insulin. If you want to use a correction dose however the timing would be at meal-times and not in-between when glucose will likely be dropping.